

To wake up on a dreary, dismal day, someday in the future, somewhere in a climate change affected world, anywhere.
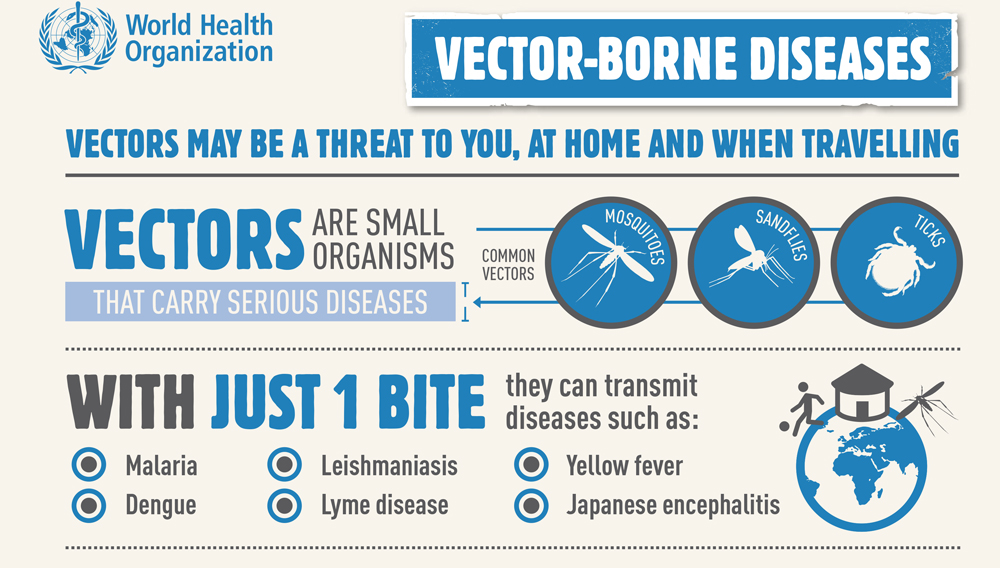
To have mosquitogenic conditions where there were none earlier, to have the double whammy of communicable diseases (led by vector borne diseases) and non-communicable diseases (heart disease, hypertension etc).
To have ‘eliminated’ diseases such as malaria, and have it back with a vengeance, to have dengue and chikungunya establishing strongholds in urban concrete jungles. And to have vintage tools and no effective medication, vaccines or prophylactics, to fight these with.
Dystopian reality.
Or, to have a future where the relentless pace of health technological innovation (HTI) has unleashed a crop of tools and interventions made available to those tasked with keeping populations healthy. High-tech tools that are responsive to emergent situations, cloud based mapping systems that proactively identify disease hotspots, Artificial Intelligence (AI)-based disease prediction algorithms relying on crowd sourced multiple input points, point-of-care diagnostics that are accessible and affordable, intelligent self-care focused bots, engineered vaccines that are agnostic to emergent variants, medications that are smart, Internet of Things (IoT) vector surveillance and identification tools, integrated vector control measures that are tailored with the environment in focus. The wish list is never ending.
What separates fiction from reality is the innovation that our bright sparks in the start-up community keep on coming up with. Some HTIs verily may be flights of fancy, with no practical application in the real world, some might have limited application by actual people, however all are usually given the funding frenzy driven marketing spiel of being ‘game changers’. To keep a brilliant inventor and more importantly, the marketers of her innovation, grounded in the reality of population level pragmatism is an unenvied burden for the behemoth that is Public Health, in its reluctance to adopt and scale up newer HTI unless ‘proven’ with a track record of ‘primum non nocere’ (first do no harm).
Do we need fancy gizmos or bleeding edge technology in dealing with a ubiquitous enemy that has been around since times immemorial? Or do we need smart deployment of HTI within the confines of a conventional, grounded approach and the resource constraints of a population level approach? Many do not appreciate that ‘feet on ground’ is often far more important than ‘head in the clouds’ when dealing with the multitude of nasty vectors that have plagued mankind possibly since humankind first walked across grassy plains and since Malaria was first recognized in the Roman civilization along the banks of the River Tiber.
At the root of proliferation of vector borne disease is the creation of mosquitogenic conditions across more locations throughout the globe, due to the at times insidious, at times overt impact of climate change, and disruptions of weather micro patterns. Increased man-vector interactions are the next, followed by a relative lack of preventive and curative means available to modern Medicine. Even though we have several promising vaccines making their way into our inventory, with the new kid on the block being the Dengue Vaccine recently licensed globally. However, the long-term efficacy on a population level is to be seen, before judgment can be passed. Treatments mostly are symptomatic for most mosquito-borne viral diseases, with drug resistance in plasmodium transmitted malaria being a major problem affecting treatment outcomes. Diagnosis too is an area of concern, with gold standard protocols being decades out of date.
Can we control, or do we need to control, a ubiquitous insect, possibly as old as mankind itself? At what cost to the environment? Do we indulge in pedantic obsequies by strategically pushing an agenda for ‘Elimination’ when in reality, there is only an illusion of control. Will HTI in vector-borne disease control, truly be a ‘game-changer’, or will it be yet another damp squib in a sky full of fireworks, as mankind deals with Climate Change?
Ideally, a systems approach is the optimum approach to deal with the needs of a healthcare ecosystem, especially when terms such as Universal Health Coverage, in a setting of Comprehensive Primary Healthcare are in vogue. Simply, it means the development of HTI solutions based on requirements that have emerged from a study of the ground realities in dealing with vector-borne diseases, with the expectations of people and those tasked with controlling such diseases being balanced. And not unilaterally developed solutions for problems which may not need addressing.
Public Health, the practice of, is more art than science. Dealing with people and their idiosyncrasies that predispose to illnesses, attempting to keep blissfully unaware populations safe and well, acting in spite of administrative apathy and a general unwillingness to accept what’s good for the greater many, working with Nature to tackle vector-borne diseases as a subset of communicable (infectious) diseases, to be a part of the solution and not a part of the problem, all of these are what Public Health deals with on a day-to-day basis.
Thus, HTI for vector borne disease control needs to be pragmatic. What may appear to be a ‘game-changer’ for a laboratory scientist, may not even be a ‘kick-off’ for a jaded Public Health practitioner.
Agencies such as the India Health Fund identify, support and scale HTIs through a pooled mechanism of health financing and incubation. A boon to innovation and to a start-ups for sure.

Col. (Dr) MP Cariappa, Technical Advisor, Public Health at Tata Trusts. Col Cariappa is a medical doctor and an ex- military Public Health Specialist with extensive experience in India and Africa over the past 30 years in vector borne disease control. He has also been a Professor at the Armed Forces Medical College, Pune.
His areas of interest and expertise in Public Health are Health Risk Communication & Health Systems Architecture.
Publication Date: 15th Dec 2022
India Health Fund is registered as Confluence for Health Action and Transformation Foundation (CHATF), a Section 8
charitable company incorporated in India, supported by the Tata Trusts.