When nations clash over competing interests and political pressures, effective leadership and local collaboration become essential lifelines. Regional cooperation and national commitments, backed by global frameworks, are vital to ensure that climate policies protect ecosystems, advance social justice, and, critically, safeguard public health. The question then becomes: How do we turn pledges and partnerships into measurable progress for both people and the planet?
The answer lies in action that bridges mitigation and adaptation integrated strategies1,2, such as decentralized solar projects in Sub-Saharan Africa that power clinics and homes while curbing deadly air pollution or mangrove restoration in Southeast Asia that shields coastal communities from storms while filtering pollutants and preventing waterborne diseases. In this way, climate solutions are thus health solutions: prioritizing initiatives that combat environmental and biodiversity threats, and protecting human well-being while building resilience against emerging disasters.
The displacement of 26.4 million people by extreme weather in 20233 is a harsh reminder of how vulnerable regions bear the brunt of this crisis. Heatwaves, floods, and storms don’t just leave destruction but expose deep inequalities in how we experience and respond to a planet under immense pressure.
Coastal areas are increasingly facing intensified flooding and storm damage, while arid regions struggle with worsening droughts and water shortages. These localized challenges call for innovative, locally-driven strategies to combat the drivers and health impacts of climate change. By investing in research, technology, and community-led initiatives, we can turn the tide on this crisis and build sustainable, healthy populations. Yet, the main challenges remain: What are the most pressing obstacles we must overcome?
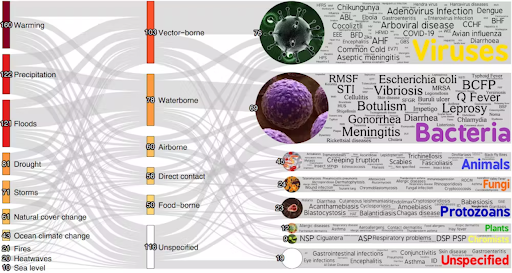
One of the greatest challenges lies in the profound health consequences of climate change, which are becoming increasingly difficult to ignore. Rising temperatures, frequent heatwaves4, and shifting weather patterns are increasing rates of respiratory and cardiovascular diseases. Warmer climates are driving the spread of vector-borne diseases (see Figure 1) like dengue and malaria, as mosquitoes and ticks expand into new regions. Flooding and extreme weather are polluting water supplies, causing outbreaks of cholera and other water-borne illnesses, while the trauma of displacement and loss is deepening a global mental health crisis. Water scarcity in many dry regions is increasing the incidence of hygiene-related diseases. The impact on agriculture is contributing to food insecurity and malnutrition, particularly in sub-Saharan Africa and Southeast Asia. These interconnected challenges emphasize the need for comprehensive solutions that tackle immediate health risks while strengthening long-term resilience5.
Health at Risk: Water, Heat and Diseases!
Heat waves, once rare, now wither cities from Ouargla to Paris, overwhelming health systems and claiming lives, increasing heatstroke, dehydration, kidney failure, and cardiovascular stress, especially in regions with limited access to water, cooling systems, or healthcare facilities. Wildfires in 2024 affected people in Australia, California, and South America, exacerbating respiratory issues already worsened by longer and stronger pollen seasons and air pollution. Rising temperatures fuel the spread of vector-borne diseases such as malaria in Kenya and Nigeria and dengue fever in Thailand and the Philippines.
Beyond immediate health threats, climate change is also intensifying less visible but equally dangerous crises. One such crisis is antimicrobial resistance (AMR)6, but how exactly does climate change fuel this “silent pandemic”? Rising temperatures are creating ideal conditions for bacterial resistance to thrive, particularly in South Asia. Warmer climates and changing ecosystems alter landscapes and reshape microbes that threaten health. Climate-induced conflicts and displacement in countries like Yemen7, Syria8, and many others are straining healthcare systems, with limited access to diagnostic and treatment, misuse, and quality of antibiotics, putting vulnerable populations at greater risk.
Figure 1: Simplified version of pathogenic diseases aggravated by climatic hazards
The increased UV exposure due to ozone layer depletion—caused by industrial chemicals that also drive climate change—is contributing to rising skin cancer rates in Australia9 and New Zealand. Extreme weather events, like recent hurricanes in the Caribbean and global wildfires, disrupt ecosystems, bringing humans into closer contact with wildlife and heightening the risk of disease spillover. Biodiversity loss, a silent companion to climate change, destabilizes ecosystems and creates new pathways for zoonotic diseases, as witnessed in outbreaks of Ebola and Marburg10 in recent years.
Regional and National Strategies for Climate Change Mitigation and Adaptation
The climate crisis, when paired with biodiversity loss – a silent companion- proves that regions that have combined mitigation and adaptation, integrating health, are seeing real benefits while addressing key areas of impact:
1. Renewable energy transition while strengthening health systems
The high cost of renewable energy is a major barrier, especially in Sub-Saharan Africa, where energy poverty hampers development and weakens health systems. Upfront investment in solar or wind projects can be costly, but alternative financing options are emerging. Take, for instance, the African Development Bank’s Desert to Power initiative, which aims to provide 10 gigawatts of solar energy to 250 million people11 in the Sahel by 2030, reducing fossil fuel dependence while promoting development.
Figure 2: The Top 10 GHG Emitters Contribute Over Two-Thirds of Global Emissions
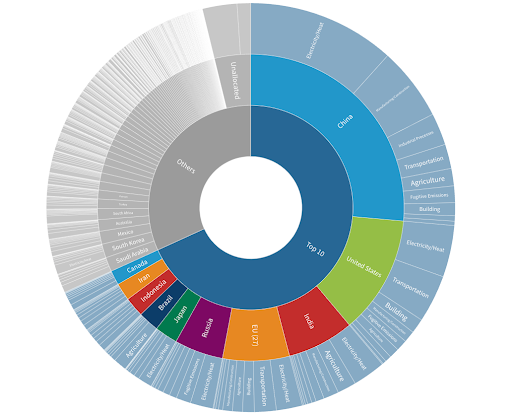
National contexts reveal the complexities of this transition. In India, electrification efforts have reduced the number of people without electricity from 400M in 2020 to 5.6M in 2021, but reliable, affordable, and clean energy remains a challenge, particularly in healthcare units12. While India is pursuing ambitious renewable projects like the world’s largest solar park in Rajasthan, coal persists to meet rising demand as shown in Figure 2. Similarly, in South Africa, the Industrial Energy Efficiency Project aims for smarter energy use to reduce emissions, lower costs, and boost competitiveness. This reflects a “both-and” scenario where emerging economies must pursue costly renewable energy and efficiency while balancing immediate economic and energy needs.
2. Early Warning Systems – region-specific and tech-driven
As climate-related health threats continue to grow, regional collaboration and early warning systems are needed to strengthen resilience in communities, enabling them to respond to emerging challenges.
In South Asia, the SAARC Disaster Management Centre’s real-time flood alerts across Nepal, India, and Bangladesh have been crucial in reducing health crises. During recent floods in Nepal, it facilitated the rapid deployment of oral rehydration salts and vaccines. Past interventions, like Bangladesh’s 2017 cyclone relief, showed significant declines in waterborne diseases when alerts were combined with swift medical action.
In Southeast Asia, the ASEAN Dengue Task Force uses an AI model13 and monsoon data to predict and prevent outbreaks. In 2023, Thailand and Cambodia avoided thousands of dengue cases by spraying larvicides in high-risk areas before peak rainfall, demonstrating the importance of integrating technology and regional cooperation to effectively combat vector-borne diseases.
Similarly, the Caribbean Institute for Meteorology and Hydrology14 provides hurricane forecasts directly to hospitals, enabling timely evacuations and resource mobilization. In the Pacific15, Fiji and Vanuatu use early warning systems that automatically shut down coastal health facilities when seismic sensors detect undersea earthquakes to protect critical coastline infrastructures.
3. One Health Approach
Brazil’s Amazon monitoring programs illustrate the power of integrating human, animal, and environmental health by using satellite tracking to identify deforestation hotspots, while field teams monitor wildlife for pathogens such as the Ebola-related Marburg virus – this made them detect an unusual die-off of bats16, prompting pre-emptive quarantines to prevent an outbreak17.
Regional strategies are key in addressing health risks that span one health approach, complex and challenging in terms of effective coordination across sectors, but once in place, they enable faster responses to emerging threats like zoonotic diseases, pollution, and biodiversity loss. In Southeast Asia and Africa, collaboration initiatives have improved disease detection and prevention while promoting stronger cross-border cooperation, such as the case of deforestation, food security, and gorilla monitoring integration in Rwanda18 and Uganda.
The growing need for health diplomacy
Local innovation and action are invaluable, yet they can only go so far. To truly address the health impacts of climate change through mitigation and adaptation, we will require health diplomacy at both regional and global levels. In a world increasingly fragmented by geopolitical tensions, where collective action becomes difficult, collective action to fill the gaps left by global inaction. Health Diplomacy can bridge these gaps by promoting data sharing and coordination, strengthening health systems, and improving information exchange. However, scaling up these efforts requires local budgets, political will, and community support, alongside overcoming challenges like data-sharing barriers and dependence on ODA to ensure long-term sustainability.
The recent “panic” surrounding the U.S.A. withdrawal from the Paris Agreement demonstrates the need for regions and nations to take the lead on climate action. As the G7 and G20 face increasing pressure to address issues such as sustainable financing, security, AMR, and mental health in climate-affected communities, regional and local solutions become more promising and essential.
Such diplomatic efforts play a crucial role in bridging the disconnect between global ambitions and on-the-ground realities, translating commitments -whether global, regional, or national – into tangible results.
When we act at local and regional levels and secure accessible, sustainable financing, robust health diplomacy becomes the cornerstone that transforms our commitments into tangible, lasting change.
