Request a proposal for developing minimally/non-invasive devices for screening or detection of tuberculosis (TB) and Vector-Borne screening. As an organization committed to advancing public health initiatives, IHF recognizes the urgent need for efficient and accurate methods to screen and detect Tuberculosis and Vector-Borne infections, especially in resource-constrained settings.

The RFP is divided into two themes: A) Tuberculosis and B) Vector-Borne Infections
Theme A: Tuberculosis: Background
Tuberculosis remains a significant global health concern, affecting millions of individuals worldwide. Traditional methods of TB screening often involve sputum-based tests, which can be time-consuming, invasive, and challenging to implement, particularly in populations with limited access to healthcare facilities. They may also lack sensitivity for early detection, leading to delayed diagnosis. Also, TB screening faces challenges due to the complexity and cost of available diagnostic tools, which require specialized infrastructure and trained personnel. Limited availability of point-of-care tests hinders screening leading to poor case notifications. It is also noticed that insufficient knowledge of TB screening guidelines leads to suboptimal screening practices. Limited Integration of screening tests into primary care workflow, is another factor resulting in missed opportunities for early detection and timely referral.
Therefore, India Health Fund is seeking innovative and non-invasive solutions that can enhance TB screening efforts and improve diagnostic accuracy.
Theme B: Vector-Borne Infections: Background
India faces a persistent endemic burden of different Vector-Borne diseases (VBD) in urban and rural areas. The distribution of VBDs in the country varies across its demography and geography, thereby leading to challenges in early and accurate diagnosis of the illness. Although 92% case reduction is noted in Malaria from 2000 to 2019, the absolute number of cases remains high at 1.6 lakh cases (2021). Moreover, there is an increasing burden of other VBDs like Chikungunya, Dengue, and Zika Virus. There is a need for strengthening the screening and diagnosis of all the existing and novel VBD burdens in the country. There is a need for building technologies that inform better decisions on treatments through screening of high-risk populations and geographies followed by early and accurate diagnosis.
Therefore, India Health Fund is seeking innovative, non-invasive or minimally invasive solutions that can enhance Vector-Borne screening and diagnostics efforts to inform appropriate and timely treatment.
Scope of Work of the RFP
The primary objective of this request for proposal (RFP) is to identify qualified innovators/suppliers/manufacturers capable of providing minimally invasive or non-invasive devices/tools/products for screening of Tuberculosis and Vector-Borne infections.
Selection and minimum eligibility criteria to ensure fitment to the proposal
The innovation should address the following criteria:
Portability and Ease of Use
The devices should employ non-invasive techniques to detect and screen for TB and Vector-Borne infections through minimally invasive sample collection methods.
Accuracy
The devices should demonstrate high sensitivity and specificity in screening TB and Vector–Borne infection ideally comparable to or exceeding the performance of existing diagnostic methods. The selected device should demonstrate strong yield and population coverage.

Non-Invasiveness or Minimal Invasiveness
The devices should employ non-invasive techniques to detect and screen for TB and Vector-Borne infections through minimally invasive sample collection methods.

Affordability
Cost-effectiveness is a critical consideration. The proposed devices should be affordable, considering the target regions and populations where they will be implemented.

Minimal Training Needs
The technology must be easy to use for end-users. The device/equipment should be easily used through minimal training for end-users.

Lab-Free Technology
The minimally invasive tools should preferably provide point-of-care test results as opposed to the requirement for complete laboratory setups.

Primary Level Healthcare
The innovation needs to be compatible to be used at the low-resource settings at the primary level of care in rural and/or urban settings.

Made In India
The selected device should be developed and manufactured in India for usage in public health programs.

Scalability
The selected devices should have the potential for scalable production and deployment, allowing for widespread adoption and impact.

Readiness
The product should be at a stage to demonstrate proof of evidence of improvement/advancements brought by the new test.
Swarms of Aedes aegypti, a warm-temperature-adapted mosquito flying over the northern most once snow-sprinkled villages near the North Pole, spreading malaria, dengue and chikungunya in remote populations that haven’t even heard of the disease, challenging health practitioners and health systems with pathogens unknown to them – all these could become reality in no time from now. And this is just one example of the devastating link between climate change and the widening spread of infectious diseases.
The climate crisis is unleashing infectious diseases – the new and the old
According to the World Economic Forum, Climate change can worsen more than half, precisely 58% of human infectious diseases[1] — from spread of hepatitis linked to flooding[2], to increased lifespans of mosquitoes carrying malaria due to warmer temperatures[3], to droughts that bring hantavirus-infected rats to human colonies in search of stored grains, to extended wet periods that facilitate increased rat populations[4]. And this doesn’t even account for the unknown diseases and pathogens yet to emerge due to climate-linked changes. For instance, thawing of the permafrost is already unearthing viruses that were once frozen in time, opening a pandora’s box of pathogens[5],[6]. And this has already started. In 2016, a 12-year-old in Siberia died of anthrax that was thawed from a reindeer carcass frozen deep below the snow[7]. The re-emerged disease sickened over 90 people and killed over 2000 reindeers. Studies are also warning the possible release of antibiotic-resistant bacteria owing to the melting permafrost[8].
While data is still emerging and studies are underway, according to one report, the largest number of diseases aggravated by climate change involved transmission by vectors such as mosquitoes[3]. Atmospheric warming or changes in rainfall patterns such as flooding and extended monsoons are altering transmission dynamics, breeding patterns, geographical range and feeding habits of mosquitoes, and thus the incidence of mosquito-borne diseases. One meta-analysis showed that overall, a 1°C rise in temperature is associated with a 13% increase in risk of dengue occurring[9]. Earth’s temperature is already 1.15°C above the 1850–1900 average[10]. A Lancet study has found that by 2070 the population at risk of malaria and dengue fever may increase by up to 4.7 billion additional people, relative to 1970–99[11]. Anopheles stephensi, a type that can carry multiple malarial parasites – plasmodium falciparum and vivax – at the same time, which was largely found in Asia, is now spreading to East and West Africa[12]. By 2050, the two main disease-spreading mosquitoes – Aedes aegypti and Aedes albopictus — will significantly expand their distribution, posing a threat to half the world[13].
Climate crisis is also indirectly impacting infectious diseases by altering human behaviors. For example, during heatwaves people tend to spend more time in water, leading to increased water-borne diseases. Cases of Vibriosis increased following periods of heatwaves in Sweden and Finland in 2014[14]. Climate-related hazards are also altering disease burden by weakening immunity, through malnutrition for example, making people more susceptible to infectious diseases like tuberculosis[15].
The infectious disease argument for climate action has not been clearer.
The call to action
On one hand, we need to put all forces forward to lower the pace of advent of climate crisis by cutting down greenhouse gas emission. On the other, we need to tackle the hazard at hand. The toll of infectious diseases linked to prolonged heatwaves, flooding, severe storms is rising by the day. We need to put immediate brakes to nip them in the bud. Below are three actionable steps:
Stronger disease surveillance
As soon as a new disease emerges or an old one reemerges, strong disease surveillance measures and radars must be in place to detect them quickly at local level and authorities must take action to stop them before the disease has had a chance to spread. Hotspot determination, disease modelling that takes into account local variations in weather along with disease dynamics will be critical[16]. Innovations like Moskeet, supported by India Health Fund and led by TrakItNow, is an AI-powered surveillance tool that can identify concentrations of different species of infected mosquitoes from their wing beats and can enable effective vector surveillance and control activities for Malaria, Dengue, Chikungunya, Japanese Encephalitis and Zika Virus.
Strengthening health systems through smarter and better diagnostics
Impact of climate change on rising burden of infectious diseases must also be tackled by strengthening health systems through making better diagnostics available to people, especially the underserved, right where they need them. Because just like COVID-19, the climate emergency will hit everyone, but it will impact the vulnerable and the marginalized first and hardest. Point-of-care diagnostic tools, faster active case finding and digital screening solutions must be accessible and available to everyone, everywhere at minimal costs, to cut down the time and cost linked to disease detection and treatment – both for patients and for health systems.
Connecting the dots and talking One Health
The recent crisis of COVID-19 and monkeypox were likely of zoonotic origin. There is an increasing consensus among the community that addressing human health issues must go hand-in-hand with animal health and environmental health. A unified “One Health” approach that values interconnectedness is a must if we are to comprehensively mitigate the impact of climate change on infectious diseases and prevent any linked future pandemics.
Financing innovations and fostering partnerships: Enablers for intersection between climate and health
Science and tech-backed innovations have the potential to address each of these above measures – stronger surveillance, better diagnostics and One Health approach. However, funding for the development and deployment of such innovations have often fallen short. Financing the development and deployment of tools that can check infectious diseases quickly and effectively will help us in a big way in tackling this human face of climate change. Funding pandemic preparedness and health systems strengthening must also take a front seat.
Strong partnerships will be the second key enabler. The mammoth task will need all stakeholders – from governments and NGOs, to private entities and communities, to collectively reinforce health systems with better tools and better prepared workforce. “Bringing together the right actors to establish integrated approaches for adaptation” is one of the key pillars laid by the WHO for building climate resilient health systems[17].
As the world gears up for the UN Climate Summit (COP28), where for the very first time in 28 years there will be a whole day on climate change’s impact on health, bringing these issues to the table will be key to making COP28 a success. Lacking which, the linked costs and consequences – for health and economics – will be hard to bear.
About the Author:
Priyamvada Chugh is a Senior Communications Manager at India Health Fund, a Tata Trusts initiative. A cancer biology researcher by training, Priyamvada has manoeuvred into public health communications owing to the power that effective communications holds for the health domain.
References:
1. Climate change is making infectious diseases worse for humans | World Economic Forum (weforum.org)
2. https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-04961-4
3. https://www.thelancet.com/journals/lanplh/article/PIIS2542-51962100132-7/fulltext
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8778283/
5. Viruses in permafrost: Scientists have revived a ‘zombie’ virus that spent 48,500 years frozen | CNN
6. ‘Zombie’ viruses are thawing from melting permafrost in Russia – The Washington Post
8. Emergent biogeochemical risks from Arctic permafrost degradation | Nature Climate Change
9. Dengue fever: the impact of increasing temperatures and heatwaves – eBioMedicine (thelancet.com)
15. Undernutrition and Tuberculosis: Public Health Implications – PMC (nih.gov)
16. Climate-proofing a malaria eradication strategy | Malaria Journal | Full Text (biomedcentral.com)
Publication Date: 29th Nov 2023
Malaria remains a significant global threat, particularly in regions with limited access to healthcare and resources, causing substantial morbidity and mortality each year. Insights on the disease’s epidemiology, emerging trends, and progress can help inform policymakers, healthcare providers, researchers, and innovators, guiding strategic interventions, resource allocation, and efforts to combat malaria worldwide. The infographic below, gives you some of the key malaria figures.
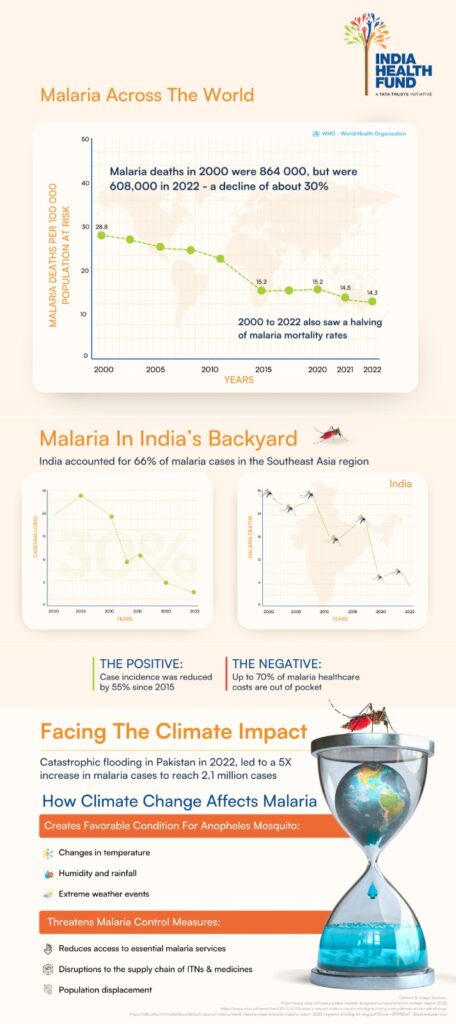
At India Health Fund, we are deeply committed to the fight against malaria and prioritize not only supporting innovations but also ensuring accessibility to data to empower individuals and organizations to develop effective solutions and drive progress in malaria control and elimination efforts.
Publication Date: 13th Mar 2024
Share
Faster, more accurate diagnosis & reporting of malaria in 1 minute with a $1 test
Problem
In the absence of an accurate, rapid diagnostic test for malaria, there are many avoidable deaths due to delayed diagnosis, specially in remote areas. Between to 2-4% of malaria cases can be missed due to genetic mutations, leading to false negatives and potentially fatal consequences for patients.
Solution
A one-minute, bivalent, accurate rapid diagnostic test for malaria, that works on a simpler principle of detecting Hemozoin, a metabolic by-product formed due to malaria infections. The hand held device tests for both Plasmodium falciparum (Pf) and Plasmodium vivax (Pv) using a single blood sample at the patients’ doorstep, with test results available in 1 minute. The targeted cost per test is $2, which is half of currently available tests. The device enables automated data capture and transmission of case & patient details to the malaria surveillance system ensuring case details are reported in real time. Gazelle is a platform which also supports a test for the diagnosis of sickle cell disease. Tests for other infectious diseases using this platform are under development.
IMPACT
While Gazelle for malaria detection is under development, it is already being used in resource-limited settings for rapid detection of Sickle Cell Disease across 27 countries worldwide including in India
“IHF has helped us continue the momentum and development of our malaria technology. They connected us with many of the top leaders/advisors in malaria in India. This group provided feedback on how to improve our project. IHF has been a real partner alongside us to work to achieve the project goal. The last 2 years were beyond anything we could have expected. We had to stop collecting data, delay the project and were unable to come to India directly. But IHF stayed with us, kept focused on the goal and that made a big difference.”
Patti White, CEO – Hemex Diagnostics
Related Articles
Faster, more accurate diagnosis & reporting of malaria in 1 minute with a $1 test
Problem
In the absence of an accurate, rapid diagnostic test for malaria, there are many avoidable deaths due to delayed diagnosis, specially in remote areas. Between to 2-4% of malaria cases can be missed due to genetic mutations, leading to false negatives and potentially fatal consequences for patients.
Solution
A one-minute, bivalent, accurate rapid diagnostic test for malaria, that works on a simpler principle of detecting Hemozoin, a metabolic by-product formed due to malaria infections. The hand held device tests for both Plasmodium falciparum (Pf) and Plasmodium vivax (Pv) using a single blood sample at the patients’ doorstep, with test results available in 1 minute. The targeted cost per test is $2, which is half of currently available tests. The device enables automated data capture and transmission of case & patient details to the malaria surveillance system ensuring case details are reported in real time. Gazelle is a platform which also supports a test for the diagnosis of sickle cell disease. Tests for other infectious diseases using this platform are under development.
IMPACT
While Gazelle for malaria detection is under development, it is already being used in resource-limited settings for rapid detection of Sickle Cell Disease across 27 countries worldwide including in India
“IHF has helped us continue the momentum and development of our malaria technology. They connected us with many of the top leaders/advisors in malaria in India. This group provided feedback on how to improve our project. IHF has been a real partner alongside us to work to achieve the project goal. The last 2 years were beyond anything we could have expected. We had to stop collecting data, delay the project and were unable to come to India directly. But IHF stayed with us, kept focused on the goal and that made a big difference.”
Patti White, CEO – Hemex Diagnostics
Related Articles
In 2024, India faced heatwaves on 28% of days during the first nine months of the year. Intensifying heatwaves are known to bring water scarcity and droughts, and have direct and indirect impacts on human health. But the impact is not gender neutral. Women and girls often bear a disproportionate impact from climate disasters. For instance, heatwaves increase the likelihoods of underweight women by 35%, child marriage by 37%, teenage pregnancies by 17% and gender-based violence by 50%.
Climate change impacts are not gender neutral
Globally, women comprise 80% of the people displaced during climate emergencies and are 14 times more likely to die during disasters, facing overall greater health risks from climate change and its devastating consequences. The increased risks women face stem from multiple access barriers including health care, education and other resources. These limitations heighten their vulnerability during and after climate-related disasters. Climate change implications can further worsen gender inequalities, reducing women’s resilience and deepening social and economic exclusion. The impact pathways of climate change on human health are intricate and complex, but to understand the higher risks for women and girls, their unique context across markets and obstacles must be examined.
Women and girls are disproportionately affected by poor access to clean water and sanitation after climate-related disasters. This lack of access ranks among the top five causes of women’s deaths globally, leading to higher rates of urinary tract infections, other bacterial infections, diarrheal diseases and menstrual hygiene issues. Prompt and safe treatments for these issues for women are often unavailable, and antibiotic misuse or increased exposure to drug-resistant pathogens escalates the global threat of antimicrobial resistance.
Substantial challenges are also encountered in accessing maternal and reproductive health care services during and after climate-related disasters. These challenges arise due to displacement, restricted access to health care facilities and disruptions in medical supply chains. For instance, in the highly flood-prone state of Assam in India, local infrastructure and facilities are often submerged and communities displaced every monsoon season. This severely restricts access to health services, leaving pregnant women and newborns particularly vulnerable. For these women, 15 Boat Clinics – mobile healthcare units on boats – operating across 13 districts in the state are the only points of care for prenatal, postnatal, neonatal and even childbirth services. However, these clinics are mostly accessible as per prior schedules as opposed to on-demand care. Such health care supply chain disruptions can also limit access to sexual and reproductive health services, resulting in unintended pregnancies, unsafe abortions, increased sexually transmitted infections and long-term consequences such as infertility.
Women and girls also often experience increased physical and mental stress as primary caregivers during adverse events. Women tend to partake in livelihoods and other responsibilities with high physical and environmental exposures, such as working in farmlands, fetching water or household cleaning and cooking. In times of climate crises, these exposures increase, advancing health risks such as vector-borne diseases, dehydration, heat strokes, or indoor air pollution. A study in Tamil Nadu, India, found that pregnant women engaging in moderate to heavy physical work had nearly doubled risks of miscarriage and adverse pregnancy outcomes due to occupational heat exposure. Climate change can further limit the educational and workforce opportunities for women and girls and increase the likelihood of child marriage and gender-based violence.
Discussions on climate and health are becoming more prominent as the number of natural disasters globally increase. However, Sustainable Development Goal (SDG) 13, which aims to address climate change and its impacts, currently does not include health- or gender-related indicators. To ensure women are protected against climate change and related disruptions to care, a comprehensive approach is required.
Gender-disaggregated data is a fundamental need for targeted and inclusive action
There continues to be a gap in the availability of gender-disaggregated data, i.e., data categorized by sex, across global and national statistics. As per the Gender Data Outlook 2024, 44% of the gender-specific data needed to measure progress on the SDGs was still missing. Recognizing the need for and advancing gender-disaggregated statistics in national programs is key to addressing gender-based health disparities, especially in low- and middle-income countries. Moreover, not only does data need to be disaggregated by gender, but also standardized in the metrics collected and granular across district, state and sub-national levels for stronger evaluation and decision-making. Mainstreaming such data requires prioritizing gender equality in data collection, analysis and policymaking. For example, one such global data alliance is working to improve the quality of and access to cross-cutting gender data. The organization is focused on addressing gaps in gender data, increasing its demand and usage, and enabling it as a lever for more gender-responsive policymaking and advocacy. Advancing such efforts for the availability of data focused on the impacts of climate change on women’s health will play a crucial role in response and resilience.
Locally-led solutions and plans that recognize gender are key
The impact of climate change on women’s health varies depending on their local contexts. Often within the same country, women and girls encounter different challenges based on varying access to food systems, housing, infrastructure, income and education opportunities, and community support. These challenges necessitate targeted adaptation-based solutions. However, national and sub-national adaptation plans and policies often do not explicitly prioritize women. For example, a study revealed 43% of state-level action plans in India did not have significant mentions of gender. A one-size-fits-all approach to climate change adaptation may not be effective. It is crucial to focus on resilience and adaptation for women’s health, tailored to their local needs and contexts.
The unique perspectives and rights of women and girls need to be heard
Women are frequently excluded from decision-making related to climate change response, which can increase their exposure to its impacts. Although there is growing awareness of the health implications of climate change, the specific challenges faced by women and girls require further attention. Including women’s perspectives in policymaking, financing, health systems strengthening, and disaster relief and response efforts is essential. For instance, the Women’s Environment and Development Organization works to incorporate women’s voices in climate change policymaking and promotes gender-responsive climate action.
Research shows that countries where women have higher social and political status generally have lower emissions and climate footprints. Women play a crucial role in climate change mitigation and adaptation. We must address the marginalization and discrimination faced by women and girls, which further heightens their vulnerability to climate change health impacts. Prioritizing gender-disaggregated data, localized resilience, and elevating women’s voices are essential in advancing more targeted research, policies, financing, leadership and community mobilization towards achieving gender equality and resilience for all.
A breakthrough RT-PCR test to speed the detection of drug resistance in TB patients from 4 months to 2 weeks
Problem
In the absence of an effective triage test for TB which can help narrow down the number of presumptive TB patients, health systems around the world have to undertake a large number of confirmatory TB tests – requiring more financial and human resources, and increased testing capacity. An accurate and affordable triage test for use at the point of care can help reduce the number of confirmatory tests required, and presumptive TB patients.
Solution
The world’s first point of care, biomarker and antibody based TB triage test, which will identify presumptive TB patients within 20 minutes at the point of care, for further confirmatory diagnosis,. This will significantly speeding up diagnosis and initiation of treatment. The test is accurate, targeting 90% sensitivity & 72% specificity and affordable, at a target cost of Rs 125 (~$1.7) per test. It will require no laboratory infrastructure, and minimal training of health care workers.
IMPACT
As the test meets an urgent national priority and holds the potential to dramatically reduce the financial burden on the national TB control programme, the Ministry of Health and Family Welfare, Government of India, is closely following developments in the project and WHO and CTD have requested to fast-track development. Furthermore, ICMR has committed to undertake multi-centric validation for Stellar’s TB triage test.
“IHF came into our project as our fairy Godmother. Not only has IHF provided us with additional funds when that were most needed, but also supported us with advice, connections and regular reviews. Their understanding of the TB ecosystem in India, and their consistent positive and pragmatic support have brought a lot of clarity on strategic approaches that could expedite dealing with the challenges in this venture.”
Suman Laal, Chief Scientific Officer and Director, Stellar Diagnostics
Industry-first innovations designed by Ameliorate Biotech Pvt. Ltd. and Medprime Technologies
Mumbai, 21 February 2023
India Health Fund (IHF), a Tata Trusts initiative focused on improving health outcomes in infectious diseases, today announced funding for two pioneering platform tools that can be used for diagnosis of multiple diseases. Developed by Ameliorate Biotech Pvt. Ltd. and Medprime Technologies respectively, the innovations, a fever panel to detect dengue, chikungunya, and malaria; and a microscope-agnostic AI-enabled diagnosis software that is applicable across diseases.
Mosquito-borne diseases are rampant in India with an observed rise in dengue and chikungunya cases between 2015 and 2021. While malaria prevalence has reduced over the last 20 years, absolute numbers stand high. These illnesses often present similar symptoms at an early stage, which can lead to a misdiagnosis or even delayed diagnosis. Thus, there is an immediate need for a rapid diagnostic test (RDT) that is real-time, easy-to-use, affordable, user-friendly and equipment free. Similarly, an algorithm that can swiftly and accurately diagnose diseases like malaria without the subjectivity that comes due to variation in skills and training of microscopists is invaluable to remote communities. Microscopy as a diagnostic tool for malaria has evolved very little since its first use.
Ameliorate Biotech Pvt. Ltd
An accurate, multiplexed RDT for dengue, chikungunya and malaria (with malaria falciparum and vivax differentiation), the simple 15-min test uses a single test kit and a single blood sample and can be easily used by minimally trained workforce at primary level. The process eliminates the need of serum/plasma samples, is instantaneous, doesn’t need cold chain facility/ biosafety lab; ensures minimal medical waste generation. The 12-month funding from IHF will enable prospective, multicentric performance and cost-effectiveness evaluation of the RDT, to be made available at a discounted price of Rs 200/pc to the public health system for government procurements. This is far less than existing fever panel priced at Rs. 3000-4000.
Dr Rashbehari Tunga, Managing Director and Founder, Ameliorate Biotech Pvt. Ltd. said, “Ameliorate has a game-changing solution at hand that can help individuals in the remotest corners differentiate quickly between fever illnesses and seek appropriate treatment”. Dr. Binita Shrivastava Tunga, Director and Co – founder, Ameliorate, added “Support and funding from India Health Fund will provide the much-needed impetus for this innovation to reach the underserved.”
Medprime Technologies
An artificial intelligence-powered software for faster, more cost-effective and more accurate microscopy for disease diagnosis deploys an algorithm, locally trained by machine learning, which automatically detects, identifies and differentiates between malarial parasites (P. falciparum and P. vivax). This tool will be microscope, disease (communicable and non-communicable) and sample (blood, urine, stool, pus) agnostic and will slash- by third- the time taken for slide viewing, image processing and result reporting. The algorithm will also overcome the need for trained manpower and will prove important for training and research for medical, paramedical and allied health staff that need remote collaboration and interoperability. IHF’s 24-month support to Medprime will enable the development and pilot testing of this AI/Machine Learning (ML)-led multiplex diagnosis software.
Samrat, CEO, Medprime Technologies added, “AI is reshaping our world. Our digital solution, backed by India Health Fund, is future-ready and will tap into the power of artificial intelligence to ensure that malaria and other diseases are diagnosed quickly and correctly, even in the most distant corners of the country, and offer an easy-to-use open design remote tool for research, training and education purposes, which is another pressing need.”
Madhav Joshi, CEO, India Health Fund said, “Empowering frontline health workers with platform tools that can test multiple diseases rapidly and accurately is bound to save lives and strengthen the national surveillance mechanism. Ameliorate’s fever panel and Medprime’s diagnostic algorithm will, through our support, be able to reach communities in most need of these advancements, working toward eliminating infectious diseases without the handicap of specific technology, geography and affordability”.
Gaining more from less, by using innovations that can diagnose multiple diseases, will not only increase efficiencies and save costs for the already-strained health systems but also save precious time for patients and allow for right treatment linkages to be made. The two IHF-supported “Made In India” tools hold the promise for just this.
About Ameliorate
Ameliorate Biotech Pvt. Ltd. is a start-up company by alumni of IIT Kharagpur and incubated at the Atal Incubation Centre, NITTE University, Karnataka. They offer early rapid diagnostics with cutting edges technology, affordable therapeutic proteins, and health supplements. Ameliorate has been awarded grants for research by KBITS for Idea to PoC, 2017, Infosys Aarohan Award, 2019, PRISM funding from DSIR, 2020 and BIRAC Jancare 2022. The company focuses on highest quality standards & business ethics which will be driven by people, research & technology. For more information: amelioratebiotech.com.
About Medprime Technologies
Medprime Technologies is a medical device company, started in the year 2014, that aims to revolutionize pathology services by creation of digital, connected and AI led pathology solutions. It was incubated by SINE at IIT-Bombay and has also received support from the likes of Social Alpha, NASSCOM, Venture Centre and has won BIRAC BIG Grant and Maharashtra Start-up Award. Medprime has launched 2 products so far: Cilika and Micalys. Cilika is the world’s first smartphone and tablet integrated microscope range that is suitable for diagnostic and research applications. The integration of smartphone technology enables digital viewing, sample image and video capture, live streaming, projection, annotation, and telepathology straight from the microscope itself. Micalys, the second product is a multifunctional digital microscopy platform which can function as a whole slide scanner, enable remote access and robotic control of the microscope for remote consultations and support ML based diagnostic algorithms. For more information: https://www.medprimetech.com/. LinkedIn: Medprime Technologies; Twitter: @medprimetech; Instagram: @medprimetech.
About India Health Fund
India Health Fund is a not-for-profit organization that was set up as a collaborative initiative of Tata Trusts and The Global Fund to Fight AIDS, Tuberculosis and Malaria. IHF’s mission is to help reduce preventable deaths from communicable diseases and other public health risks. IHF does this by de-risking the development of promising technology and science-led solutions that have the potential to make a significant difference in the diagnosis, treatment, and prevention of these diseases. IHF collaborates with the public and private sectors to facilitate the development, adoption, and scaling of these solutions. IHF’s aim is to improve health outcomes, with a focus on primary care and in low resource settings. For more information, please visit https://www.indiahealthfund.org. LinkedIn: India Health Fund Twitter: @IndiaHealthFund. Instagram: @india_health_fund.
About Tata Trusts
Since inception in 1892, Tata Trusts, India’s oldest philanthropic organisation, has played a pioneering role in bringing about an enduring difference in the lives of the communities it serves. Guided by the principles and the vision of proactive philanthropy of the Founder, Jamsetji Tata, the Trusts’ purpose is to catalyse development in the areas of health, nutrition, education, water, sanitation and hygiene, livelihood, digital transformation, migration and urban habitat, social justice and inclusion, environment and energy, skill development, sports, and arts and culture. The Trusts’ programmes, achieved through direct implementation, partnerships and grant making, are marked by innovations relevant to the country. For more information, please visit http://tatatrusts.org/. LinkedIn: Tata Trusts Twitter: @tatatrusts Instagram: tata_trusts.
———
For more details, please contact:
Current Global Jeunelle Rebello +91-8806749170 |
Publication Date: 4th January, 2024
Key Media Coverages

Mumbai, 13 December, 2022
India Health Fund (IHF), a Tata Trusts initiative, today announced its funding and support for a first-of-its-kind lollipop- and chewing gum-inspired sputum collection device for testing tuberculosis (TB) among children. Being developed by 221B Biomedical Pvt. Ltd., and christened ‘Blow-Pop’, it will help address lakhs of under-, mis- and delayed diagnosed cases of TB among children. The unique child-friendly sample collection device is expected to be ready for roll-out over the next two years.
Every year, 1-1.151 lakh children get affected by TB in India. Of these, 96%2 of deaths, among paediatric TB patients, are due to a lack of bacteriologic confirmation and early treatment. These missed cases not only contribute to higher mortality but also increased transmission of infection in communities. Exacerbating this, are current sample collection methods, which are time-consuming, painful and inconvenient for children and often need the expertise of healthcare workers.
- Nearly 1 – 1.15 lakh children in India get affected by TB every year. Thousands of cases go unmissed as the testing is not child friendly. Current sample collection methods are painful, time consuming and inconvenient.
- First-of-its-kind sample collection device to be developed by 221B Biomedical Pvt. Ltd. with grant and support from India Health Fund, a Tata Trusts initiative.
- The flavoured low-cost device will require children to simply chew and blow or cough for easy and safe sample collection of oral fluids.
- The innovation will make testing simpler and will likely increase testing and treatment rates, lower mortality and infection transmission due to TB.
Addressing this unmet need and keeping children at the heart of the innovation, India Health Fund’s latest grant to 221B Biomedical will pave the way for development and clinical validation of 221B Biomedical’s simulated method. The innovation is a low-cost device that will improve the safety, efficacy, and ease of sputum collection for TB in children. Inspired from a lollipop, and chewing gum user experience, the conch-shaped device needs children to simply chew and blow or cough for easy sample collection of oral fluids. Moreover, owing to its simplicity, the tool will be ideal for low-resource settings, including primary healthcare setups. While this tool will be developed initially keeping children in mind, a similar product can be used among adults too, and its development and deployment will be explored.
 “Today’s announcement brings fresh hope for thousands of children who are missing out on TB testing because sample collection is not child friendly,” said Madhav Joshi, CEO, India Health Fund. “Making the testing process simpler and pain-free will increase rates of testing and diagnosis, leading to fast-tracked treatment initiation and preventing unnecessary deaths in children. Moreover, it will also reduce expenditure for patients and health systems alike.”
“Today’s announcement brings fresh hope for thousands of children who are missing out on TB testing because sample collection is not child friendly,” said Madhav Joshi, CEO, India Health Fund. “Making the testing process simpler and pain-free will increase rates of testing and diagnosis, leading to fast-tracked treatment initiation and preventing unnecessary deaths in children. Moreover, it will also reduce expenditure for patients and health systems alike.”
He further added, “Accessibility and high impact potential is a key feature that is common to all innovations funded and supported by the India Health Fund because an innovation is only as powerful as it is accessible.”
 “Innovating while keeping children at the center of our work is likely to bring smiles for lakhs of little ones and their caregivers. The power of this innovation lies not only in its affordability, safety, speed and convenience for children, but also in its compatibility and complimentary to existing diagnostic setups at minimal costs,” said Dr. Vivek Manoharan founder & CEO, 221B Biomedical Pvt. Ltd., India.
“Innovating while keeping children at the center of our work is likely to bring smiles for lakhs of little ones and their caregivers. The power of this innovation lies not only in its affordability, safety, speed and convenience for children, but also in its compatibility and complimentary to existing diagnostic setups at minimal costs,” said Dr. Vivek Manoharan founder & CEO, 221B Biomedical Pvt. Ltd., India.
1. ‘Invest to End TB. Save Lives!’ – Press release by MoH&FW, Govt of India
2. The global burden of tuberculosis mortality in children: a mathematical modelling study – The Lancet Global Health.
About 221B Biomedical Pvt. Ltd
221B Biomedical Private Limited (221B) aims to simplify medical diagnostics for easy and convenient home-based testing experience with its proprietary, scientific and innovative technologies. 221B aspires towards a diagnostics first approach, while proactively anticipating and preventing diseases in an effort towards progressing the UN sustainable development goal (SDGs) on health and well-being. 221B is an associate of Test At Home Private Limited, Singapore, an Antler portfolio company, supported by National University of Singapore and UNLEASH global innovation lab for SDGs. 221B is founded by a duo of a biomedical engineer scientist and a medical doctor: Dr. Vivek Manoharan (BEng, MS, PhD) & Dr. Terence Tan (MBBS, GDFM, GDOM).
About India Health Fund
India Health Fund is a not-for-profit organization that was set up as a collaborative initiative of Tata Trusts and The Global Fund to Fight AIDS, Tuberculosis and Malaria.
IHF’s mission is to help reduce preventable deaths from communicable diseases and other public health risks. IHF does this by de-risking the development of promising technology and science-led solutions that have the potential to make a significant difference in the diagnosis, treatment, and prevention of these diseases. IHF collaborates with the public and private sectors to facilitate the development, adoption, and scaling of these solutions. IHF’s aim is to improve health outcomes, with a focus on primary care and in low resource settings. For more information, please visit https://www.indiahealthfund.org.
LinkedIn: India Health Fund Twitter: @IndiaHealthFund. Instagram: @india_health_fund
About Tata Trusts
Since inception in 1892, Tata Trusts, India’s oldest philanthropic organisation, has played a pioneering role in bringing about an enduring difference in the lives of the communities it serves. Guided by the principles and the vision of proactive philanthropy of the Founder, Jamsetji Tata, the Trusts’ purpose is to catalyse development in the areas of health, nutrition, education, water, sanitation and hygiene, livelihood, digital transformation, migration and urban habitat, social justice and inclusion, environment and energy, skill development, sports, and arts and culture. The Trusts’ programmes, achieved through direct implementation, partnerships and grant making, are marked by innovations relevant to the country. For more information, please visit http://tatatrusts.org/
LinkedIn: India Health Fund Twitter: @IndiaHealthFund. Instagram: @india_health_fund
———
For more details, please contact:
|
India Health Fund Priyamvada Chugh priyamvada@indiahealthfund.org +91-8130640487 |
Current Global Jeunelle Rebello +91-8806749170 |
Key Media Coverages
Submission of Proposal
Applicants are required to submit proposals to India Health Fund with details as requested in the application form. Applicants should specifically mention the expected support from IHF:

Objective of Support
Mention the support expected from India Health Fund with a clear description of the need and what the support would enable.

Budget and Timeline
Propose a realistic timeline for the development, manufacturing, and delivery of the devices, considering any clinical or regulatory requirements.
Submission and Deadline
Create an account on the Manthan platform and submit your applications here along with requisite attachments a) proposal form and b) budget sheet no later than 8th September 2023. Any additional supporting documents or relevant materials should be included as separate attachments.
Detailed proposal template and budget template are available on the submission portal.
Evaluation
Applications qualifying under the scope of the proposals will receive:
- Milestone-based financial support for product development, clinical validation studies, and pilot/feasibility studies for a duration of 12 - 15 months.
- Ecosystem and network access to resources from IHF and its partner organizations.
- Mentoring and guidance from technical and business experts on product development, regulatory requirements, and market access.
All submitted proposals will be evaluated based on their technical merit, cost-effectiveness, scalability, and the organization’s track record.
Evaluation Criteria
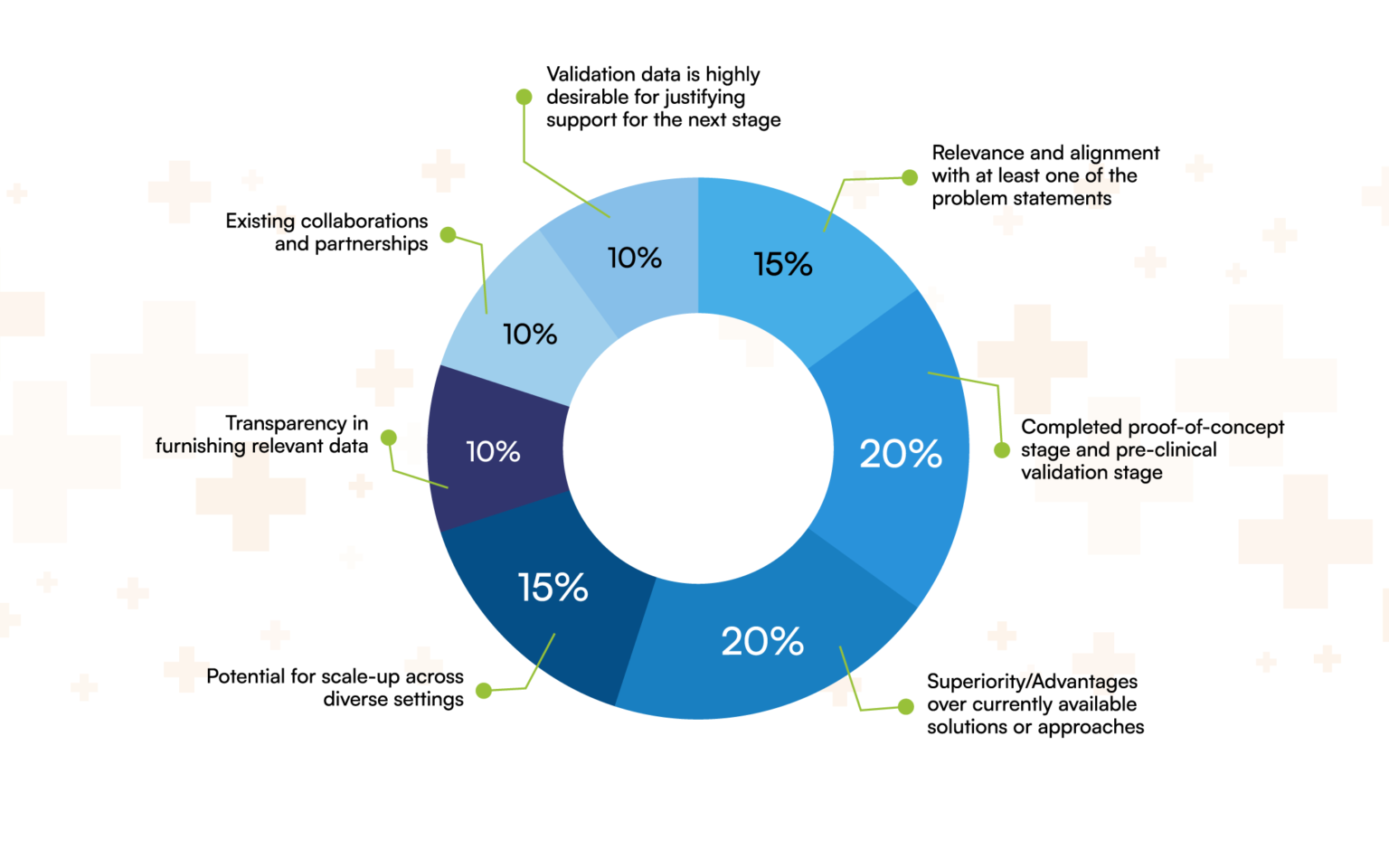
Minimum Eligibility
- Applications must be submitted by registered and incorporated entities in India.
- The proposal is relevant and aligned with requirements of the proposal.
- The innovation should have completed the proof-of-concept and pre-clinical validation stage.
- Validation data is highly desirable for justifying support for the next stage. Transparency in furnishing relevant data in support of the proposed innovation should be agreeable by the applicant.
- The innovation should be at Technology Readiness Level – 4 to 6 and should have pilot clinical data as proof of the proposed hypothesis.
- The innovation should bring superiority or incremental addition over existing methods/ tools/ devices/ assays used in primary care settings to address the problem highlighted in the scope of the proposal.
- The innovation should have the potential for scale-up across diverse settings.
The following fall outside the scope of the RFP and will not be supported by IHF:
- Basic science research
- Epidemiological studies/surveys/disease burden analysis
- Proposals focused on pure service delivery.
- Innovations in the ideation/ proof-of-concept stage/ formative studies
- Applications that propose incremental solutions without a clear innovative element
- Non-alignment with national goals of the Government of India.
- Non-alignment with the Sustainability Development Goals (SDGs) related to healthcare.
Partners